 Sepsis (Septicemia) is a reaction to severe infection. It can involve many different parts of the body. The germs causing the infection can be bacteria, viruses or fungi. It’s tricky to recognize. My research came across this fantastic British site that really drills down into sepsis, its threats — and its treatments.
Sepsis (Septicemia) is a reaction to severe infection. It can involve many different parts of the body. The germs causing the infection can be bacteria, viruses or fungi. It’s tricky to recognize. My research came across this fantastic British site that really drills down into sepsis, its threats — and its treatments.
What is sepsis?
Sepsis is a reaction by the body to severe infection. You may also hear severe infection being referred to as septicaemia. Strictly speaking, septicaemia is an infection of the blood, whereas sepsis refers to the whole body. The germs involved in sepsis can be bacteria, viruses or fungi (the plural of fungus). If bacteria multiply and release poisons (toxins) into the blood it can cause serious illness.
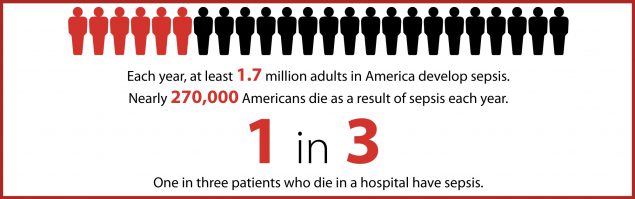
How common is sepsis?
About 1 in 500 people develop severe sepsis in England every year. The number is much higher in developing countries.
Who is at risk of sepsis?
- The old (>75 years) and the very young (< 1 year).
- People who have had surgical procedures.
- People with indwelling lines or catheters.
- People who drink alcohol excessively.
- People who inject recreational drugs.
- People who have diabetes mellitus.
- People who have had severe burns.
- People who have problems with their immune system (the bodily system that fights infection).
- Medications – eg, high doses of steroids, some medicines to treat cancer.
- Men are more likely than women to develop sepsis, although the death rate in women is higher. The reason for this is not known.
- Pregnant women.
How do you develop sepsis?
Rarely, a germ overcomes the body’s immune system, resulting in sepsis. No one knows why this happens but there are various theories. It is not clear why a few people are prone to serious illness and many other people are carriers of the same germ but have no ill effect.
Usually the germs are bacteria but sometimes they can be viruses or fungi. Studies suggest that the level of steroids in the body, the effects of various other chemicals and hormones and the way the body’s cells handle invading germs may all be involved.
What are the symptoms and signs of sepsis?
The symptoms of sepsis can be very vague. You should always seek urgent medical advice or get straight to hospital if you think you or someone close to you may have sepsis.
Symptoms are the feelings/sensations you experience when you have an illness (for example, pain). Signs are physical features. You may notice them yourself or they may only become obvious when a doctor examines you (for example, a rapid heartbeat).
Not everyone will have typical symptoms or signs. For example, the very old or very young and people who have problems with their immune system can develop unusual features and this can make diagnosis more difficult.
Symptoms
- The first thing you may notice is a symptom of the original infection. Examples would be a cough (throat or chest infection) or pain when you pass urine (urinary tract infection).
- You may feel generally unwell and, even if you have been taking antibiotic medication, your infection may rapidly worsen.
- You may develop tiredness, sickness, stomach pains or runny stools (diarrhoea).
- Later on, you may develop symptoms elsewhere in your body when the infection spreads to these areas – for example:
- Inflammation of the tissues around the brain (meningitis), due to spread to the covering of the brain.
- Kidney problems.
- A liver condition.
Signs
- You may develop a high temperature (fever) or an unusually low temperature.
- Your hands and feet may become cold and clammy, even if you have a raised temperature.
- Your heart rate may rise.
- Your blood pressure may drop.
- Your breathing rate may be higher than normal.
- You may become confused.
- You may develop blotching of the skin.
- Various blood tests may show inflammation in the body or problems with the working of organs such as the liver or kidneys.
See also the separate leaflet called Adult Sepsis Safety Net.
Children
The symptoms and signs for children may be even more vague than for adults. Children with sepsis may:
- Feel abnormally cold to touch.
- Have patchy (mottled) skin and bluish colour to the skin, or may have very pale skin.
- Have a rash that does not fade with pressure.,
- Breathe more quickly than usual.
- Be very tired and be difficult to wake up from sleep.
Young children may not want feeds, may repeatedly be sick (vomit) or may not pass any urine and so not have wet nappies.
See also the separate leaflet called Child Sepsis Safety Net.
What is the treatment for sepsis?
Sepsis is a medical emergency and treatment needs to be started as soon as possible. Always seek urgent medical advice or get straight to hospital if you think you or someone close to you may have sepsis.
- If you develop sepsis you can become severely ill. You will need to be admitted to hospital and will probably need to be admitted to an intensive care unit.
- You may require oxygen through a tube in the windpipe.
- You may need fluids through a drip directly into a vein in your arm.
- Other medicines can be given through the drip, including antibiotics and insulin.
- If pus has collected anywhere in the body, a surgical operation may be needed to drain it.
What is the outlook (prognosis) for sepsis?
The outlook for sepsis can be good if it is diagnosed and treated early. However, without early treatment, between 10 and 50 people out of 100 will die, depending on the severity of sepsis. Older people tend to fare less well, especially if they have a long-term illness like diabetes or heart disease.
Complications can include:
- Disseminated intravascular coagulation – this means the formation of blood clots in the small blood vessels throughout the body.
- Failure of the adrenal glands (the glands that sit on top of the kidneys that produce adrenaline, steroids and other important body chemicals).
- Multiorgan failure – this means that several organs of the body stop working properly. These can include the heart, lungs and kidneys.
Post-sepsis syndrome
As with any severe illness which needs intensive treatment in hospital, people recovering from sepsis may experience physical and psychological difficulties and these difficulties may last for several years.
Physical problems may include feeling very tired, muscle weakness, feeling short of breath, chest pains, fluid swelling (oedema), joint pains, poor appetite, disturbed vision, skin numbness or pins and needles, and frequent illness caused by further infections.
Psychological difficulties may include feeling anxious, feeling low or depressed, nightmares, poor sleep, poor concentration and problems with memory.
Can sepsis be prevented?
Maintaining a healthy lifestyle will reduce your chances of developing infections that can lead to sepsis. Both smoking and alcohol increase the risk.
If you have a condition which qualifies you for flu and pneumonia immunisation jabs (for example, if you have diabetes or asthma) make sure you take up these options. Children need to be up to date with their vaccinations, particularly Haemophilus influenzae type b (Hib), group C meningococcus, pneumococcus and mumps.
Produced in collaboration with Dr Ron Daniels of The UK Sepsis Trust.
